Tissue Engineering at the Children’s Hospital Zurich
The body’s own tissues can be artificially generated from its` individual cells. This approach can be used to treat congenital malformations in children, such as spina bifida, bladder malformations and large skin defects.
At the University Children’s Hospital Zurich, various groups are researching methods of using artificially produced tissues from the body’s own cells to treat malformations, diseases or large-area skin injuries in children. The following three projects will be presented in further detail at the booth.
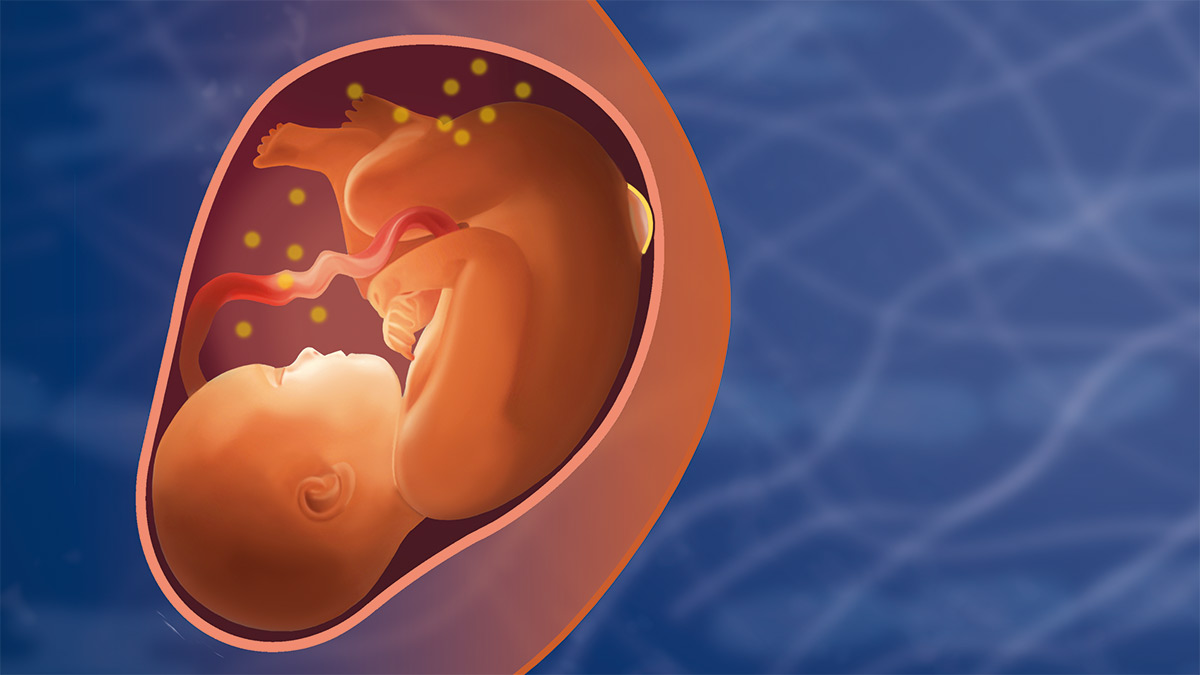
Helping the Unborn Child
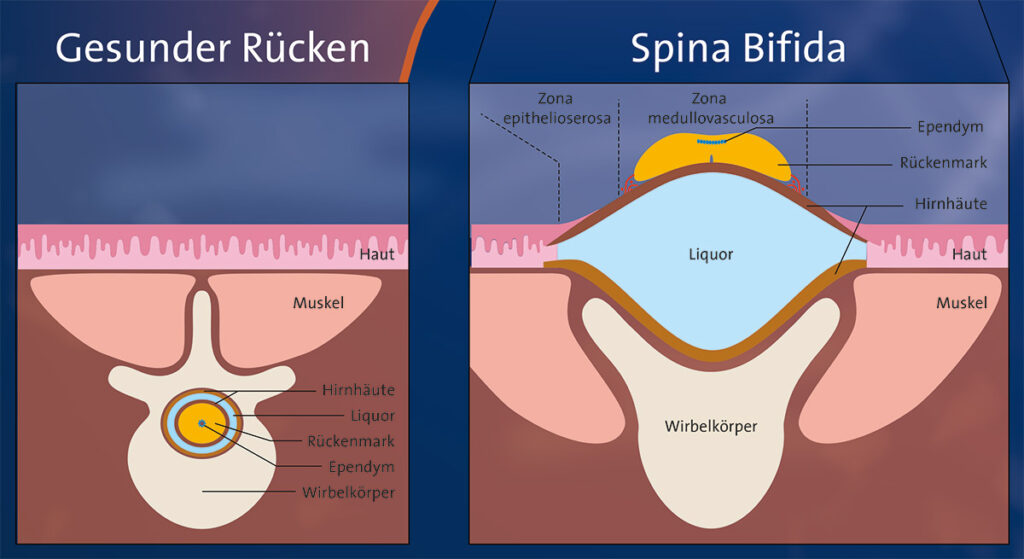
Spina bifida is a severe neurological malformation, if left untreated, it leads to considerable physical and mental disabilities. Today, fetal surgery is the state-of-the-art treatment option to yield the best possible outcomes. With the help of autologous tissue engineering and modern robotics, this therapy will be further developed and improved upon.
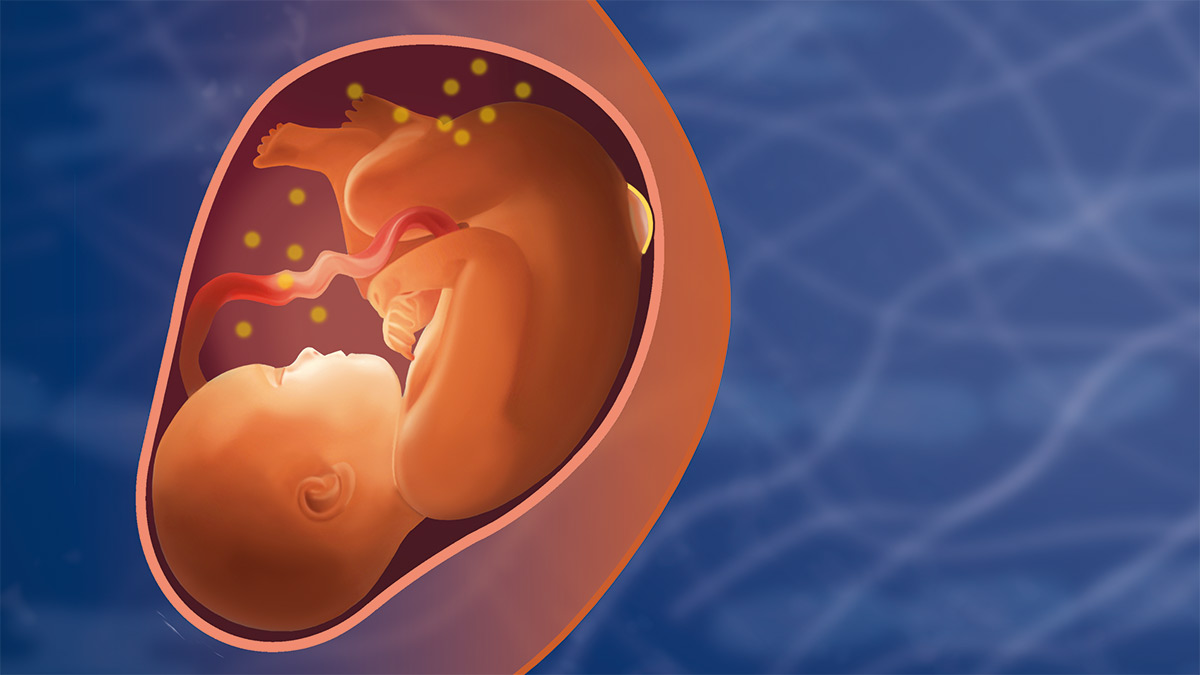
As part of routine prenatal diagnostics, an amniocentesis is performed in the pregnant woman. In addition to the cells required for diagnostics, stem cells are also obtained for subsequent tissue engineering.
These stem cells are identified and differentiated in the laboratory. Differentiation is controlled in such a way that various skin and cartilage cells can be developed from the undifferentiated stem cells. The corresponding skin and cartilage composites are grown in the laboratory and then assembled into tissue using novel cell biology techniques.
In the future, fetal surgeons will be able to implant a personalized, complex tissue construct available at the time of fetal surgery to cover the defect in the fetus and thus “re-establish” normal anatomy.
Reconstructed Skin
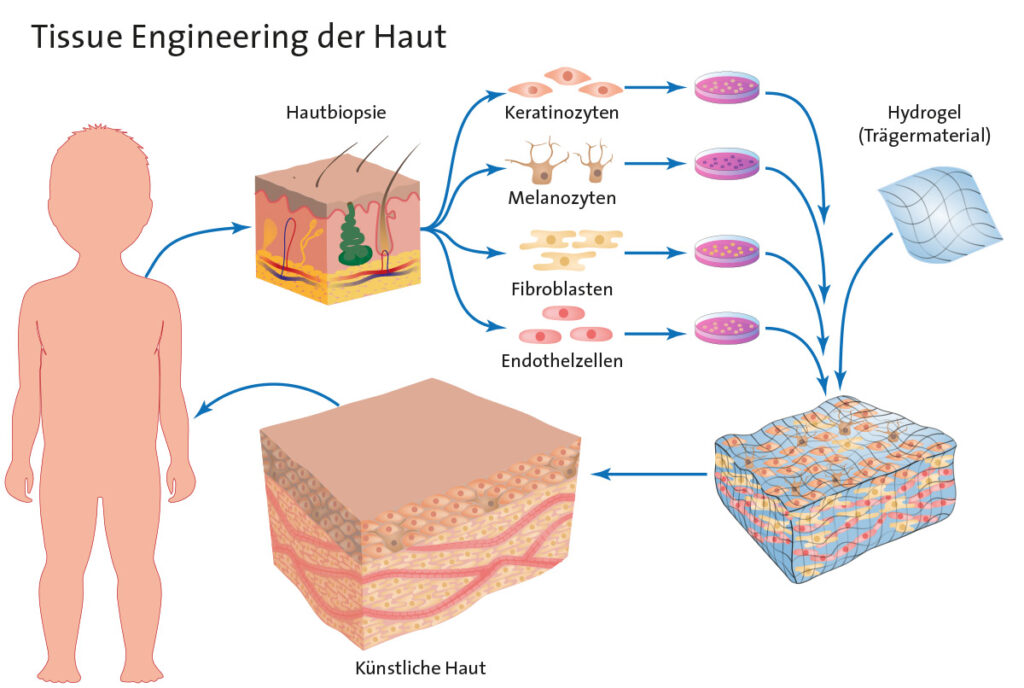
To artificially engineer skin tissue, four different cell types from a small sample of a patient’s skin are isolated in the laboratory, cultured and then reassembled as “natural artificial” skin. This way, any amount of skin can be produced.
The skin is the largest organ of the human body and shields us from damaging influences. If we injure our skin, this protective layer is missing. If the injury is extensive, as can be the case with a burn or scald, life can be endangered. The missing skin surface must then be replaced. The standard method is to graft the patient’s own skin.
However, if too much of a patient’s skin surface is injured, the remaining healthy skin cannot be used for skin grafting. In this case, a life can only be saved by growing a large area of skin in the laboratory from a small piece of the patient’s intact skin and applying this “tissue engineered skin to the patient.
For 20 years, our research team at the Children’s Hospital Zurich has been working to develop and improve on this method. In the first phase, skin with 2 cell types, the cells of the epidermis (keratinocytes) and the cells of the dermis (fibroblasts), were produced. This skin is already being used in clinical trials and is showing early success. However, since this skin does not contain all components of normal skin, the team at the Children’s Hospital Zurich is working on developing it further. Blood vessels and pigment cells are now also isolated and cultivated from the small sample of healthy skin. These 4 cell types are reassembled to recreate skin that even takes on the patient’s skin color.
Constructing the Bladder
Congenital malformations and diseases of the urinary tract impair bladder function. In severe cases, even the kidneys can suffer permanent damage. The treatment of choice is surgical enlargement of the bladder with tissue from the intestine.
In the future, it should be possible to use the patient’s own bladder tissue – thanks to “tissue engineering”, with such tissue produced in the laboratory.
Our research projects therefore address the central question of which factors promote bladder regeneration, so that the engineered tissue can restore the function of the urinary bladder after implantation in the patient.